Reconsidering migraine control and seizing the possibility of life without limitations
Lindsey experienced her first migraine when she was just 6 years old. The attacks intensified in her teen years, becoming so frequent and debilitating that she missed much of her senior year of high school. Now 28 years old, the Washington, D.C., resident manages her migraine with medication and a strict sleep and exercise regimen. She’s mindful of environments that might trigger an attack and avoids them.
This is Lindsey’s normal, but she sometimes wonders what her life would be like if she didn’t have to live around migraine—enjoying a glass of champagne at a wedding without fear that it would send her to bed for days, being able to travel more, participating in life fully and shedding the worry about when her next attack will strike. “I think a lot of people with migraine adjust and learn to live with lowered expectations,” she says. “I get about four migraines a month, and I think that’s alright, that’s good enough. But really, it’s not.”
Lindsey, a former Lundbeck employee, is one of the 39 million people in the United States living with migraine.1 No two migraines are alike, and Lindsey’s experience with migraine is unique. But her acceptance of migraine-related limitations is not, says Roger Cady, MD, a headache specialist.
“Some people become resigned and accept that they’re not going to be able to do some of the things they want to do. But it doesn’t have to be that way.”
— Dr. Roger Cady
While there have been significant advances in migraine treatment, he explains, many people with migraine still experience symptoms and lack lasting control. That’s because over time, medications to treat migraine attacks may become less effective or wear off between doses.2 And some people’s migraines worsen and become more frequent as a result of the very medications they are taking to treat their attacks. This is called medication overuse headache, or MOH.3 “After trying medications that don’t provide full relief, some people become resigned and accept that they’re not going to be able to do some of the things they want to do. But it doesn’t have to be that way,” Dr. Cady adds.
Conduct a quality-of-life check-up
This Migraine and Headache Awareness Month, Dr. Cady encourages all people with migraine to reexamine how the disease is impacting their quality of life and ask if their current treatment plan allows them to live the life they desire. Are migraine symptoms or anxiety about what might trigger the next migraine causing them to miss out on important life events? Are they making accommodations and compromises in daily life? What would they do if they could prevent migraine from occurring in the first place?
“It puts into context how many excuses many of us make about things being ‘not that bad,’ when really it’s impacting my life. I’m just used to it.”
— Lindsey
Dr. Cady urges people to consider more than just their pain level or number of headache days. Migraine deeply affects peoples’ emotional lives and can increase chances of mental health challenges. In fact, according to research, people who live with chronic migraine (defined as 15 or more headache days per month, including at least eight migraine days) are 205 percent more likely to experience depression and 140 percent more likely to experience anxiety than those who have migraines periodically.4
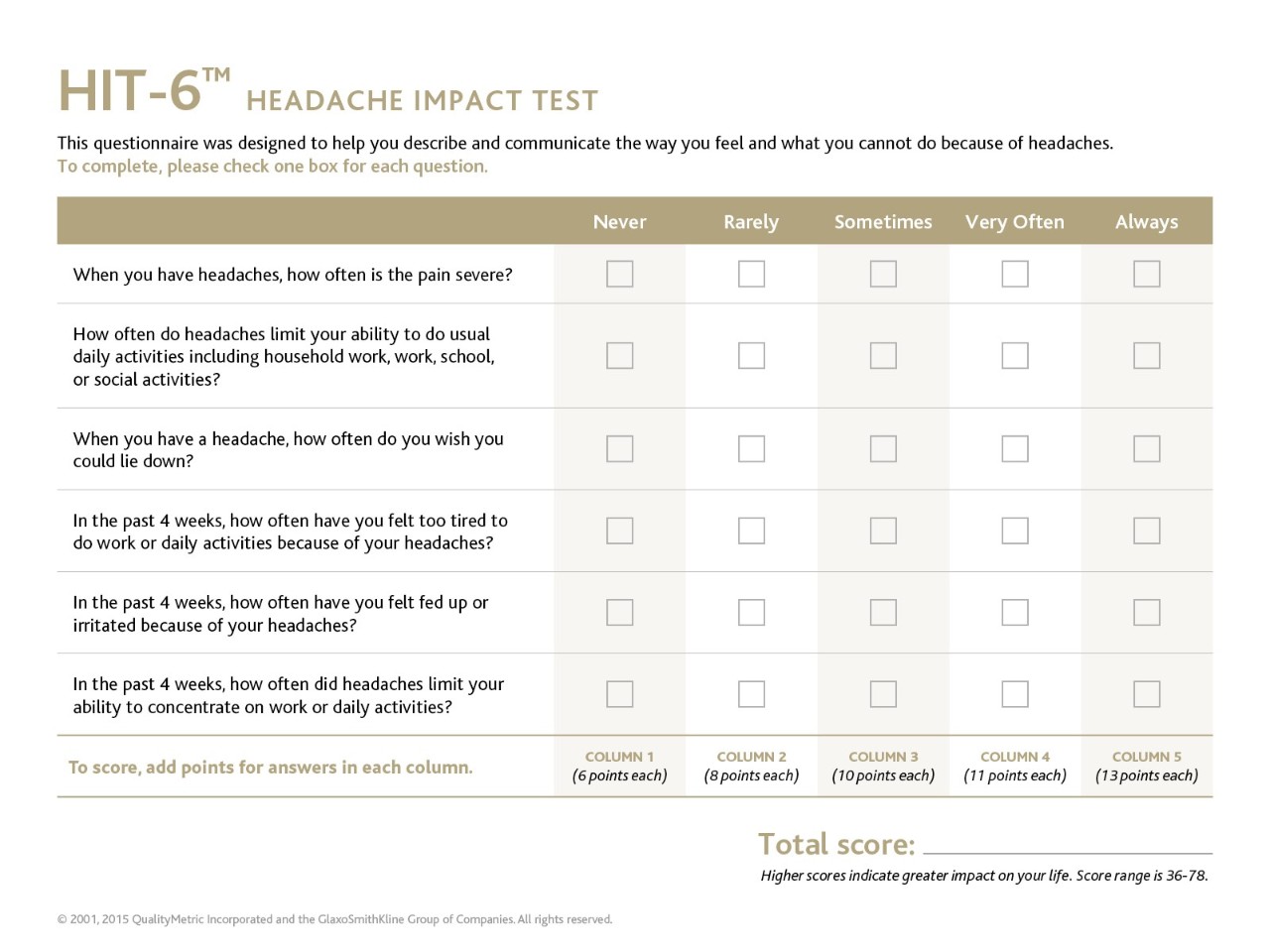
One tool that people can use to evaluate the impact headaches have on quality of life is a simple six-question survey known as HIT-6. This clinically validated tool is designed to help people communicate how they feel and describe what they cannot do because of their headaches. The survey includes questions around pain, but it also asks how often headaches limit daily activities; how often people feel fed up or irritated due to headache; how often headaches limit the ability to concentrate on work or daily activities; and how often people feel too tired to work or do daily activities because of headaches.
“It puts into context how many excuses many of us make about things being ‘not that bad,’ when really it’s impacting my life. I’m just used to it,” Lindsey says.
Trust your healthcare provider, work as a team and be proactive
According to Dr. Cady, people with migraine can use the HIT-6 questionnaire to initiate discussions with their healthcare provider about their quality of life and current treatment. Then, providers and patients can together develop a plan that works toward more-complete symptom control.
“Don’t give up hope,” says Dr. Cady. “Trust your healthcare provider, work as a team and be proactive in managing your migraine. If you treat this disease with the option that is right for you, you can live the life you deserve.”
Speak to your doctor about how migraine impacts your day-to-day activities and what treatment options might be right for you.
Sources
1. Migraine Research Foundation. Migraine Facts. Available at https://migraineresearchfoundation.org/about-migraine/migraine-facts/. Accessed April 2020.
2. American Migraine Foundation. Understanding Chronic Migraine. Available at https://americanmigrainefoundation.org/resource-library/understanding-migrainechronic-migraine-2/. Accessed June 2020.
3. 8.2 Medication-overuse headache (MOH) - ICHD-3 The International Classification of Headache Disorders 3rd edition. Available at https://ichd-3.org/8-headache-attributed-to-a-substance-or-its-withdrawal/8-2-medication-overuse-headache-moh/. Accessed June 2020.
4. Adams AM, Serrano D, Buse DC, Reed ML, Marske V, Fanning KM, Lipton RB. The impact of chronic migraine: The Chronic Migraine Epidemiology and Outcomes (CaMEO) Study methods and baseline results. Cephalalgia. 2015; 35(7):563–578.
©2020 Lundbeck. All rights reserved. UBR-C-100233 June 2020